World Sleep Day 2024: Can sleep apps drive high performance?

Dr. Jazz Croft
14 March 2024

Content
- What we know so far
- The state of global mental health research
- Unmind’s sleep research program
- Scaling up our science
- References
Getting enough sleep can be challenging for many of us, with estimates that a third of the workforce gets less than seven hours of sleep a night.1 This has a big impact on employee health and performance, with the US alone losing an equivalent of 1.23m working days due to insufficient sleep every year.2
Improving sleep quality is a powerful way to support good mental health,3 manage stress,4 and boost wellbeing at work.5 With employees struggling with sleep, and the subsequent impact on workplaces, it’s a public health and economic imperative to build science-backed, scalable support to help prevent mental health challenges and support wellbeing.
One promising field aiming to combat this problem is sleep apps. With around 10,000 apps on the market, employees have many options to help boost their sleep. However, with the explosion in app use in recent years, the scientific research needed to test the efficacy of apps and minimize harm to users is lagging behind the market.
In this article, we look at the gaps in sleep research, why the lack of investment in mental health research is a problem for the workforce, and how Unmind are tackling this knowledge gap – including our current program led by PhD student Jessica Vazzaz, funded by Unmind, the University of Sussex and the Economic Social Research Council (ESRC).
What we know so far
While digital cognitive behavioral therapy (CBT)6 has been found to effectively improve insomnia, there’s a lack of research on other popular digital tools to use before or during sleep (e.g. meditation, soundscapes, night stories).
Despite so many apps using these methods, little investment has gone into the science of their approach. With experts calling out sleep apps that risk harm, breach data privacy or are ineffective, more research is needed to support responsible innovation.7
Across digital sleep tools, evidence for their efficacy so far is mixed. While numerous studies show that relaxing music can improve sleep quality,8 we know less about whether specific sounds (e.g. white noise) or training around sleep skills are effective.9,3
The state of global mental health research
This lack of knowledge isn’t just bad news for employees, it has major consequences for organizations. Research shows poor sleep is a risk factor for burnout, mental health challenges and increased sickness absence, with fatigue-related productivity losses estimated to cost $1,967 per employee annually.10
Despite the public health and economic concerns associated with poor sleep and mental health difficulties, it’s an underfunded area of academic research worldwide. While the wellness market is valued at $5.6tn,11 95% of mental health research funding is from governments and, compared to other areas of health, mental health is underfunded.12
Globally, around $3.7bn a year is spent on mental health research, equivalent to less than 50 cents per person.
With the gap between tech innovation in the wellbeing market and scientific research into mental health support widening, solutions are entering the market without scientific research to test their efficacy, having a knock-on effect on the quality of support available to the workforce.
Unmind’s investment in research on preventative tools for better sleep and mental health addresses a key knowledge gap and supports the academic community. By investing in a PhD program, Unmind is helping researchers gain the skills to build a career tackling priority research areas in health and wellbeing.
Unmind’s sleep research program
To innovate our science-backed sleep tools, Unmind’s in-house Science team has been conducting research in collaboration with the University of Sussex to test the effects of sleep tools in scientific trials and with client populations.
Like any great TV show, our sleep research program started with a pilot. Like pilot TV episodes, pilot studies help inform bigger-scale projects, trial approaches and collect feedback. Unlike TV, our pilot is a Randomised Controlled Trial (RCT) that studies how feasible Unmind’s sleep tools are for regular use and their impact on wellbeing.
We found evidence to support that using Unmind’s sleep tools (which include bedtime stories and calming sleep sounds) a few nights a week over four weeks was feasible, easy and posed minimal risk to users.
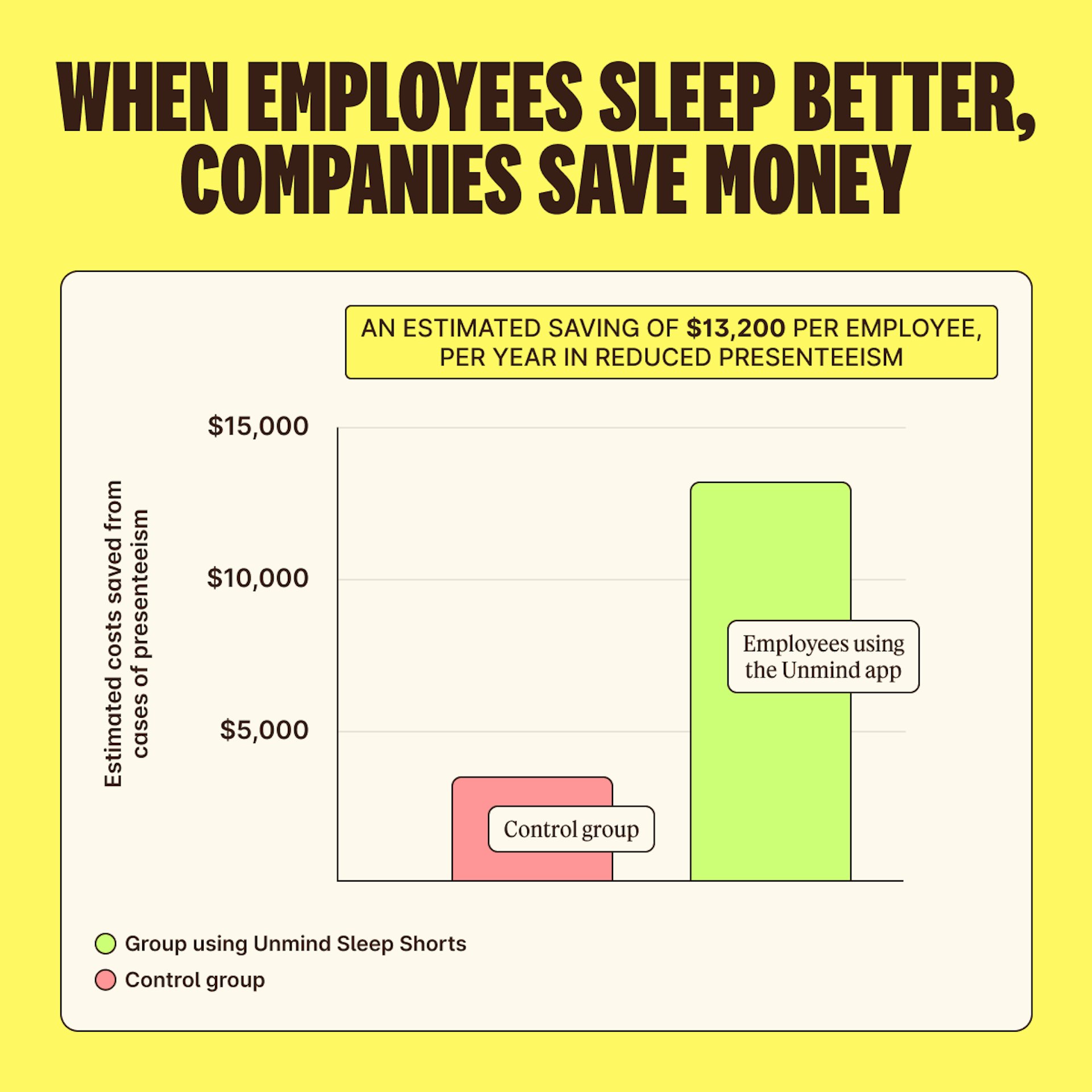
We also saw improved sleep, better mental health and better performance at work, which equate to cost savings for employers thanks to improved productivity. You can read more about our study here.
Scaling up our science
Thanks to the positive findings from our pilot study, we’re now delivering a more definitive RCT to replicate and develop our previous findings.
As part of Jessica Vazzaz’s three-year research PhD program, which includes supervision and mentorship by Unmind’s Science team, we’ll explore these key questions through a large RCT and a lab-based study investigating:
- What are the ‘active ingredients’ in digital tools that improve sleep?
- What can we learn about sleep interventions by using wearables to track sleep?
- What are users' experiences, and what can we learn from them?
By investing in the future of digital mental health research, we support the research community and sustainable, science-backed product development.
To find out more about how our science-backed platform can support sustainable high performance, book a call with an Unminder.
With support from Unmind, the PhD program is an exciting opportunity to collaborate, learn and develop as a researcher in both industry and academia.
References
1. Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of Healthy Sleep Duration Among Adults – United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(6):137-41. doi:10.15585/mmwr.mm6506a1
2.Hafner M, Stepanek M, Taylor J, Troxel WM, van Stolk C. Why Sleep Matters – The Economic Costs of Insufficient Sleep: A Cross-Country Comparative Analysis. Rand Health Q. 2017;6(4):11. doi:10.7249/RR1791
3. Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving Sleep Quality Leads to Better Mental Health: A Meta-Analysis of Randomised Controlled Trials. Sleep Med Rev. 2021;60:101556. doi:10.1016/ j.smrv.2021.101556
4. Choi DW, Chun SY, Lee SA, Han KT, Park EC. Association Between Sleep Duration and Perceived Stress: Salaried Worker in Circumstances of High Workload. Int J Environ Res Public Health. 2018;15(4):796. doi:10.3390/ ijerph15040796
5. Peng J, Zhang J, Wang B, He Y, Lin Q, Fang P, Wu S. The Relationship Between Sleep Quality and Occupational Well-Being in Employees: The Mediating Role of Occupational Self-Efficacy. Front Psychol. 2023;14:1071232. doi:10.3389/ fpsyg.2023.1071232
6. Ye YY, Chen NK, Chen J, Liu J, Lin L, Liu YZ, Lang Y, Li XJ, Yang XJ, Jiang XJ. Internet-Based Cognitive-Behavioural Therapy for Insomnia (ICBT-i): A Meta-Analysis of Randomised Controlled Trials. BMJ Open. 2016;6(11):e010707. doi:10.1136/ bmjopen-2015-010707
7. Al Mahmud A, Wu J, Mubin O. A Scoping Review of Mobile Apps for Sleep Management: User Needs and Design Considerations. Front Psychiatry. 2022;13:1037927. doi:10.3389/ fpsyt.2022.1037927
8. de Niet G, Tiemens B, Lendemeijer B, Hutschemaekers G. Music-Assisted Relaxation to Improve Sleep Quality: Meta-Analysis. J Adv Nurs. 2009;65(7):1356–64. doi:10.1111/ j.1365-2648.2009.04982.x
9. Riedy, SM, Smith, MG, Rocha, S, & Basner, M. Noise as a Sleep Aid: A Systematic Review. Sleep Medicine Reviews. 2021;55(1)101385. doi:10.1016/ j.smrv.2020.101385
10. Rosekind MR, Gregory KB, Mallis MM, Brandt SL, Seal B, Lerner D. The Cost of Poor Sleep: Workplace Productivity Loss and Associated Costs. J Occup Environ Med. 2010;52(1):91-8. doi:10.1097/ JOM.0b013e3181c78c30
11. Global Wellness Institute, Statistics and Facts https://globalwellnessinstitute.org/ press-room/statistics-and-facts/. Published 2024.
12. Woelbert E, White R, Lundell-Smith K, Grant J, Kemmer, D. The Inequities of Mental Health Research (IAMHRF). https://doi.org/10.6084/ m9.figshare.13055897.v2. Published 2020.
About the Author

Dr. Jazz Croft, Senior Scientific Liaison
About the Author
